The immediate postpartum period is a rush of pride, pain, love, hormones, new identities and again … a constantly changing body.
Below are some unglamorous tips from a pelvic floor physio to give you a 1% easier ride through this beautiful, messy journey.
The first poo … this glorious feat is required to occur before being released, by the hospital, back to the wild. You cannot lie about whether you have/haven’t, your midwife will always know (lie detection is a requirement of their registration or so I’ve been told?). Hot tips for this process include:
A. Laxitives: It is so ok to take these if you feel you need them. The hospital will have a supply. Especially useful if you are at all; nervous, tend towards constipation, in pain, tired, have haemorrhoids or feel as though your insides are falling out of you. If you feel none of the above post birth, congratulations, you are most likely a unicorn and do not need to continue reading the rest of this blog for mortals.
B. When prepping for aforementioned feat, it can be useful to bundle toilet paper, put your hand between your legs, and apply upward pressure to your perineum (zone between vagina and anus) throughout. Don’t think about it too hard, just do it, you won’t regret it – sometimes a girlfriend’s gotta do what a girlfriend’s gotta do.
C. If you happened to have been graced with a trophy (stitches, episiotomy, vaginal graze, vaginal tear) from darling child, a wet wipe can be a better tool for point B than toilet paper. Use whatever feels right to you.
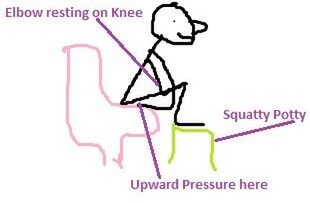
Correct positioning for your first motherhood poo:
- Rest elbow not involved in step B on your knee.
- Use a “squatty potty” AKA a step to raise knees above hips when seated. Doesn’t need to be designer, worst case a full roll of toilet paper under each foot can do (provided you are reading this post Corona virus apocalyptic panic buying and toilet paper is available again).
- Relax your stomach or ‘blow it out’. Breath out, don’t hold your breath. Don’t push, take your time.
- Take your own nice toilet paper (go on, treat yourself to the best of the best, just this once). Hospital toilet paper is average, trust me, have tried for an extended period of time, 3/10, would not recommend.
Artwork 1 of the 2020 Happy Perineum Series:
I call this … Happy Pooing
(Only Mum tells me how beautiful my artworks are … not sure how no one else sees it?)
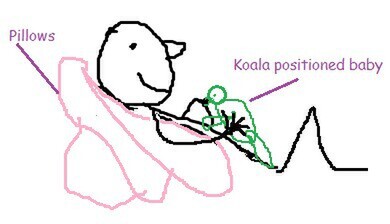
Lie down on the job to breast-feed. Try propping yourself up with pillows behind your back. Feel free to have munchkin placed across your body (traditional feeding) or laying vertically on your stomach (this is called koala feeding, cute name huh!).
Artwork 2 of the 2020 Happy Perineum Series:
Semi-Reclined Breastfeeding.
- Your trunk is horizontal, therefore you are placing less pressure on your perineum.
- You are supporting but not holding the weight of you baby … which equals happier mum wrists.
- The Pillows support your upper back/shoulders/neck … which equals no slumping forward and less visits to see me for ‘breast feeding back’.
When grazes and acid don’t mix … In other toilet related news, here’s my step by step guide to reducing the sting associated with the first few wees.
Take your own wee magic – AKA Ural. This product alkalises urine, making it significantly less stingy to pass urine. Hospitals sometimes supply this for you, but why take the risk when you can buy it over the counter at the pharmacy?
This is one of the times when pelvic floor physios recommend weeing in the shower. Just for the first little while if there’s burn and if you feel like it.
Filling a drink bottle with water and pouring this down your vulval area whilst weeing. Be kind to yourself, these extra steps are worth the effort.
The “how to reduce risk of wetting pants guide”: to start with … it is VERY normal to not have 100% bladder/bowel control immediately post birth. This does not mean that you never will have control again, or if you are experiencing this should do nothing about it. The female body’s capacity to heal post birth is AMAZING and so most of these issues sort themselves out with time and occasionally, a bit of hard work.
These tips are general and useful for the majority of women (but not all of you). If something happens during your birth process and your situation becomes a bit more specific, please seek help. Don’t be embarrassed to talk to your GP/Midwife/Pelvic Floor Physiotherapist about anything. Guaranteed whatever your symptoms are is not the first time we’ve heard of them. I talk wees, poos, sex, and babies all day … what a job!
You want me to squeeze and lift what????
The pelvic floor muscles are a group of muscles which have two main jobs:
1. The superficial muscles help to contract the diameter of your vagina and anus.
2. The deep muscles help to lift the pelvic organs upwards (towards your head).
These muscles are essential for preventing urinary leakage (1 in 3 women experience this), wind leakage or poo leakage (1 in 8 people leak faeces at least once a month). What I would recommend for everyone is getting to know how their pelvic floor muscles feel when they both contract AND relax them.
~ There is too much of a good thing when it comes to pelvic floor muscle strengthening. Being able to relax a muscle is just as important as being able to contract it. If you don’t feel like you can relax your pelvic floor, this is one of the symptoms of a condition called overactive pelvic floor. Treatable yes. Optimal for you? No. ~
Regardless of your stage of life, “get to know these guys now”. The better your brain knows your pelvic floor muscles, the quicker and stronger it will find this rock-star muscle group after giving birth.
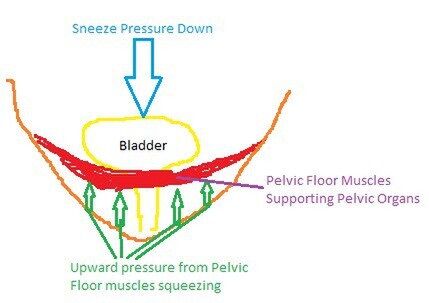
Using “The Knack”.
“The knack” is a cute term we use to describe contracting your pelvic floor muscles before, and holding throughout, a sneeze/cough/laugh/lift.
Artwork 3 of the 2020 Happy Perineum Series:
“The Knack”
Artwork 3 of the 2020 Happy Perineum Series:
“The Knack”
But really, the knack is the ticket to help prevent many girlfriends from (what some commercials refer to as) ‘light bladder leakage’. It also happens to be a whole lot cheaper (by that I mean free!) than a lifetime supply of incontinence pads (And really, who wouldn’t prefer to spend this money on their indoor plant addiction instead?).
By ‘lifting’ your pelvic floor muscles you are helping to brace the pelvic structures against downward pressures, therefore reducing the risk of losing bladder control. Do the work, practice coordinating this now, master before d-day, and use from here on in.
For the love of pinot noir, DO NOT do crazy exercise for AT LEAST the first six weeks post birth.
If you are planning on crazy exercise, I would 1000% recommend you seeing a pelvic floor physiotherapist first. We are not against exercise at all – we love it! And we want you, and your body, to love it in time.
We are however, against women’s organs falling outside of them unnecessarily due to societal pressures to be #summerbodready #postbabybodin6weeks.
~ Farmers know cows/mammals/humans look different before/after birth. Celebrities/trashy mags apparently haven’t caught onto this yet? (Is this new information? Has it been buried or locked away somewhere)? The farmers know what’s up, get your info from them instead of say … celebrity families whose last name may or may not begin with a K. Just a thought. ~
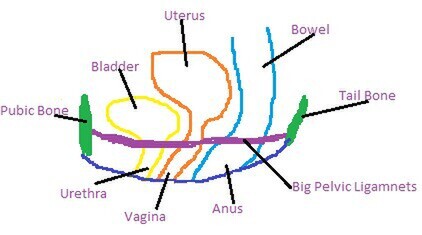
Seriously, rest now and make it your job to rest. You have strong, thick pelvic ligaments which support your pelvic organs. These get stretched during pregnancy and vaginal delivery, it is natural. Whilst it is normal for them to stretch, they believe it is normal for us to rest them afterward to allow for their optimal healing. They have big jobs to do. Love them first, exercise the rest of you later.
Artwork 4 of the 2020 Happy Perineum Series:
Your Insides Side-View
If you exercise too vigorously in this early window, you risk further irreparable stretch of these ligaments. This is results in prolapse. I treat it all the time. TBH majority of women who have had children have a degree of prolapse which just happens as a part of birth/life AND YOU CAN LIVE A PERFECTLY NORMAL LIFE WITH THIS (before hyperventilation sets in). I’m not saying this to scare you, simply to let you know if this does happen to you, you are not alone. If you had the choice though … you’d prefer less prolapse right? If I had the choice I’d choose less severe prolapse too – if that sways your decision making at all?
If you feel like exercising anywhere from week 2-6 … great! You go girl! Appropriate exercise in this early stage includes things like: light walking, stretching, yoga (with the exception of inversion type movements until you have well and truly finished bleeding), pilates … TBH, meditation and napping is also classed as exercise in this little window … Some official researcher said that I’m sure?
If you are AT ALL worried, I would always recommend you visit a Women’s Health Physiotherapist who can do internal examinations. If you are rural or don’t have access to one, there are many (including myself) who do telehealth appointments as well to chat about what you are experiencing and what needs to happen from there. Ask your midwife, there could be one at your local hospital as well.
No problem is too small, we would much prefer to check that everything is going A-OK than hear you stressing (yes health professionals can ‘hear’ stress from the waiting room 😉).
May the force be with you new mothers, we are your people, we are here to help if you need us.