What age were you when you first read in a magazine, sitting at the hairdresser, that Kegels were ESSENTIAL for living?
As essential as good Italian takeaway? Particularly if at some point, in the very obscurely distant future, you had for a split second pondered the idea of becoming pregnant. And don’t get me started on menopause, because if you had not started an Olympic level Kegel training regime by then you were definitely “a goner”.
Well…what if I told you that Kegels were not the whole story? What if I told you that there was a little bit of technique involved in a “squeeze”?
Or that some women’s muscles are constantly contracting and they need to learn how to RELAX their muscles before they can FEEL a squeeze?
Or that some women may have the world’s best muscles but their connective tissue is damaged and THAT’S why they’re leaking?
As a pelvic floor physio, I’m stoked that Kegels have been a way for us to help raise awareness of some of the things which happen “down there”. In the same token though, I wonder whether this message tells a story of muscle squeezes fixing everything, when in fact, they can’t.
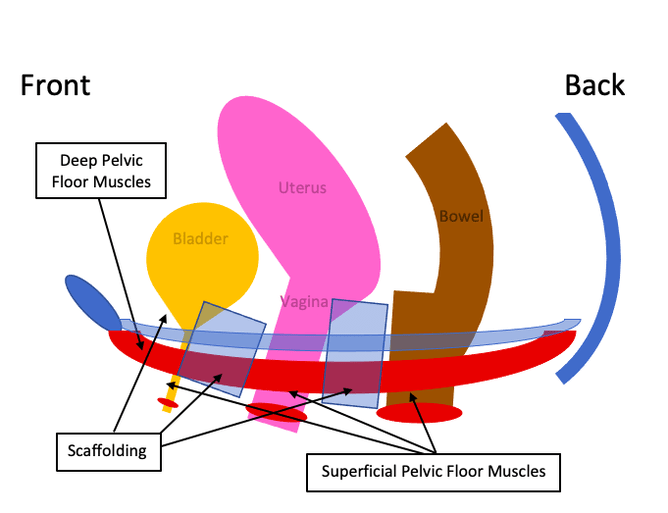
On that note, let’s explore the idea that a pelvis has both “scaffolding” AND muscles which both have a role in keeping everything working optimally. (Thank you Microsoft Word for sponsoring this original, definitely not to scale, diagram):
Scaffolding: (I come from a long line of tradies, it’s my only excuse for using this word) AKA ligaments + fascia, is what forms the structure or the “shape” of the insides of the pelvis. Scaffolding helps to keep organs up and exit shoots (urethra, vagina and rectum) running in their own lanes…winner! If the scaffolding stretches and softens a bit, we call this prolapse. Prolapse comes in stages, with a little bit of stretching being Stage 1 and a lot a stretching being Stage 4.
If damaged scaffolding is what is causing problems for you, no amount of muscle strength can fix this. Because the female body is AMAZING there is a percentage of these women whose muscles, when coordinated enough, can compensate for damaged scaffolding. If you do not fall into this percentage though, fear not, we have other tricks up our sleeve to treat scaffolding which has “seen better days”.
Deep Pelvic Floor Muscles: AKA “The lifters”.
Superficial Pelvic Floor Muscles: AKA “The squeezers”.
Who is at risk of damaged scaffolding?
Contrary to popular belief, women who have had a vaginal delivery are not the only population who are at risk of prolapse. Other risk factor include:
- Athletes (yep, the strongest of the strong!), if you are leaking or experiencing other prolapse symptoms with jumping/running/heavy lifting etc. this can and should be fixed!
- Pregnant women: increased load (+/- increased vomiting L ) = increased strain on scaffolding.
- Overweight women.
- Women with chronic respiratory conditions e.g. bronchiectasis, cystic fibrosis.
- Women with connective tissue disorders e.g. Ehlers-Danlos Syndrome.
- Women with chronic constipation/straining.
- Especially anyone who has had a vaginal delivery with or without forceps, a heavy baby or a baby with a large head circumference, posterior births, if the second stage of your active labour lasted above two hours or if you had grade two perineal tears—bonus points if you tick more than one of those boxes!
What would you feel if you did have a prolapse?
Well, this is a tricky one. Our insides are not made of steel and bricks, hence some movement is natural and normal. What we really focus on is when YOU feel that “something is just not quite right”.
Common symptoms which YOU can look out for include:
- Heavy, dragging feelings inside the vagina. Interestingly these sometimes only appear in the afternoon/evening or following high-intensity exercise. Regardless, this feeling should be investigated.
- Leaking (could be a little, could be a lot) with a sneeze, cough, laugh, jump, lift (we call this stress urinary incontinence). This can also include not being able to control your wind or bowel.
- Feeling like you don’t empty your bladder fully or needing to stand up, do a jiggle and then sit back down to fully empty your bladder.
- Difficulty passing a bowel motion.
- Seeing/feeling a “bulge” in the vagina.
- Inability to keep a tampon in.
Why should we seek help for these intimate problems?
Prolapse is super treatable, super common (~10% of women have a symptomatic prolapse) and can really impact on the quality of a woman’s life.
There are many different treatment options that we can tailor to suit you and your lifestyle. With a bit of management, symptoms can often be relieved and the rate of prolapse progression reduced.
Last but not least (Sing it with me now!)
Pelvic floor muscle squeezes:
- Do not have anything to do with tightening your tummy, butt, back or legs. They definitely do not look like a glute bridge (AKA a shoulder bridge).
- Do not involve a “bearing down” or Valsalva movement.
- Should not be painful.
- Should involve squeezing both “the front” e.g. vaginal opening and “the back” e.g. squeezing the anus.
- And with perfect technique, should involve two movements where the first feels like you are “squeezing” the diameter of your vagina smaller, before then lifting towards your head.